Reassessing the Programmed Lower Rate Limit for Cardiac Resynchronization Defibrillators-A Commentary
Authors: Arjun Sharma1*, Brian Olshansky2, Bruce Wilkoff3, Mark Richards4, Paul Jones5, Nicholas Wold5, David Persbacher5
1Unaffiliated Reno, USA
2University of Iowa, Iowa City, USA
3Cleveland Clinic, Cleveland, USA
4Yakima Valley Medical Center, Yakima, USA
5Boston Scientific, St. Paul, USA
*Correspondence to: Arjun Sharma, 1365 Meridian Ranch Drive, Reno, Nevada 89523, USA; E-mail: sharmarjun@gmail.com
Received: February 11, 2022; Accepted: February 28, 2022; Published: March 10, 2022
Copyright: © 2022 Sharma A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ORCID:
AS: 0000-0002-6484-1250
BO: 0000-0002-6044-045X
BW: 0000-0001-8905-9233
MR: 0000-0002-2197-6956
PJ: 0000-0001-5231-5563
NW: 0000-0002-1401-6893
DP: 0000-0002-7859-7834
Citation: Sharma A, Olshansky B, Wilkoff B, Richards M, Jones P, Wold N and Persbacher D (2022) Reassessing the Programmed Lower Rate Limit for Cardiac Resynchronization Defibrillators-A Commentary. 21st Century Cardiol, Volume 2 (2): 118
Abstract
The programmed lower rate limit (LRL) has not previously been associated with the survival of subjects with cardiac resynchronization defibrillators (CRT D). We hypothesized that lower LRL programming is independently associated with survival, and LRL and heart rate score (HrSc) are associated. All dual-chamber CRT-D devices in the Remote Patient Monitoring (RPM) ALTITUDE database (2006-2011) were queried. Baseline HrSc was defined as the percentage of atrial sensed and paced beats in the tallest 10 beats histogram bin early post-implant. LRL was assessed during repeated RPM uploads. Relationships between LRL, survival, HrSc, and other variables were evaluated. Survival was determined via Death Indices. Analyzed data included 61,881 subjects (mean follow-up: 2.9 years). LRL ranged from 40 to 85 bpm. Baseline lower LRL was associated with younger age, less atrial fibrillation, female sex, and lower HrSc (p<0.001 for all covariates). Lower LRL was associated with improved survival with LRL-40 bpm associated with the largest survival benefit. This was significant for all three HrSc subgroups (p<0.001). An interaction between HrSc and LRL was observed; with the largest survival difference between HrSc groups observed at LRL-40(p<0.001). Thus, LRL programming and HrSc were associated, and lower values of both were associated with improved survival in a large database of CRT-D subjects. Relationships between survival, LRL programming, and HrSc merit a controlled prospective study.
Keywords:
Cardiac resynchronization defibrillators; Lower rate limit; Histogram; Atrial fibrillation; Heart rate score
Abbreviations
AF: atrial fibrillation; CRT-D: cardiac resynchronization defibrillator; HrSc: heart rate score; LRL: programmed lower rate limit; RPM: remote patient monitoring; PPM: pulses per minute
Introduction
Despite exhaustive research regarding the programming of cardiac resynchronization therapy defibrillators (CRT-D), no consensus exists concerning the appropriate lower rate limit (LRL) for such devices. Clinicians often find themselves in a conundrum whereby they would consider chronically programming a higher LRL to improve cardiovascular functioning, but this approach may be incorrect.
Data from our studies with more than a decade of analytic research has focused on a need to reassess the programmed LRL [1]. This process was initiated by software systems engineers (D.P.) analyzing uploaded data from defibrillators in the INTRINSIC RV defibrillator trial [2]. A machine learning software program analyzed this massive data file for predictors of survival. The most powerfully predictive parameter derived from the device data was a novel parameter related to the atrial histogram, the Heart Rate Score (HrSc). This was defined as the height (in the percentage of all beats) of the tallest 10 beat/minute bin in the atrial paced and sensed histogram (Figure 1). To assess this new predictor a much larger device database was studied to assess the reproducibility of these initial findings. This larger database was the implanted device remote follow-up database (ALTITUDE 2006-2011) from Boston Scientific. 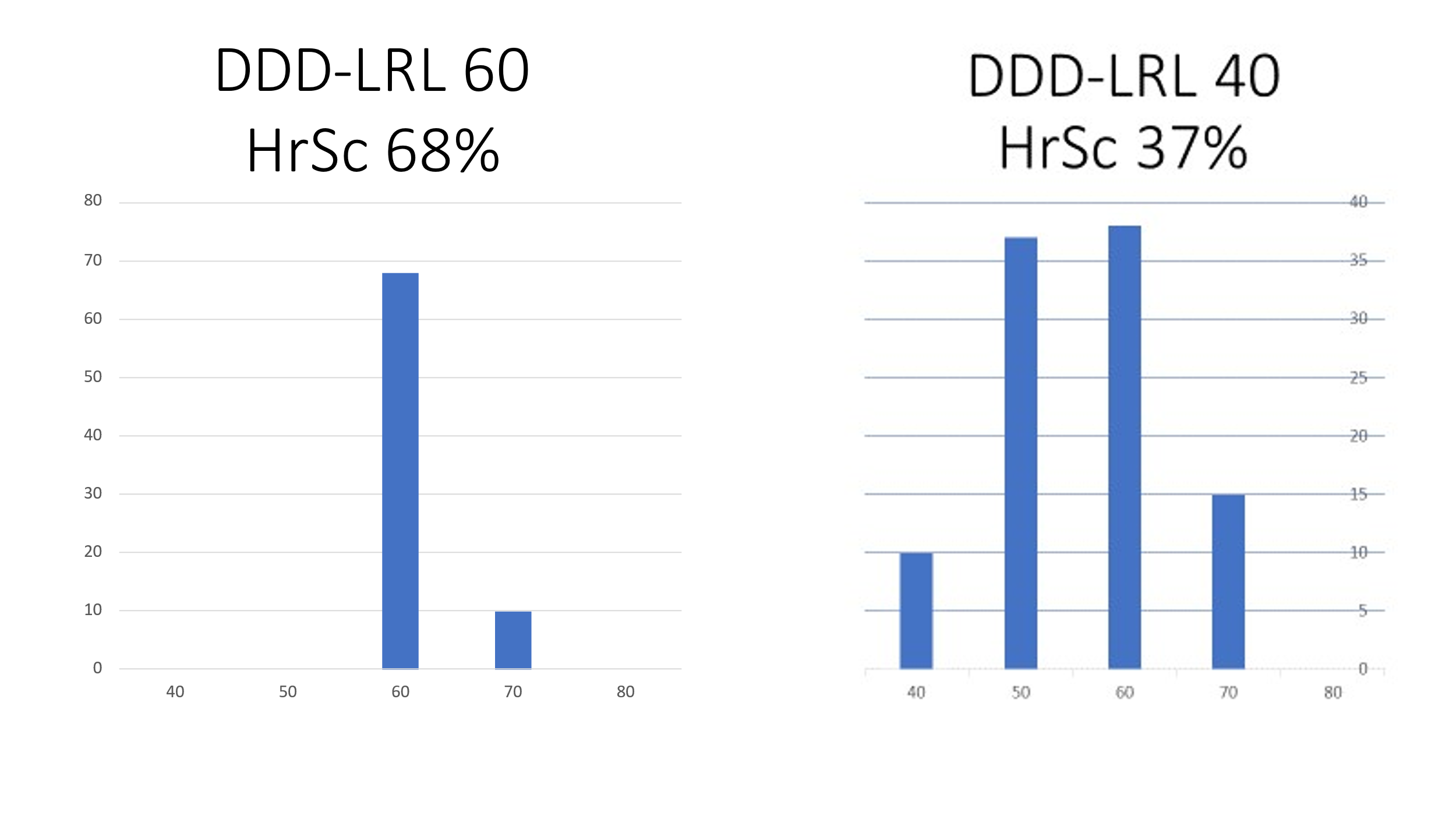
Figure 1: CRT-D Atrial rate histograms illustrating the effect of LRL on the rate. Panel A shows LRL 60 with HrSc 68% (height of tallest bin). On the right Panel B with LRL 40, lower spontaneous rates are seen, and the rates are more widely distributed, and HrSc = 37%. The vertical axis is different in the two panels, with the scale doubled on the right.
In a multivariate analysis utilizing this database, Wilkoff BL, et al. (2107) [3] showed that lower survival was associated with increasing age, presence of atrial fibrillation, male gender, and lower percent left ventricular pacing (Table 1). Prior prospective clinical trial data support the association of these parameters with survival and tends to validate this analysis. However, Wilkoff also found increasing HrSc and LRL were predictors of lower survival. HrSc and LRL were conspicuous as, in CRT-D trials, these parameters were not previously described to be associated with survival. The HrSc is based on the atrial histogram, and, as the LRL is programmed higher, the atrial rate histogram changes in a detrimental way to ultimately affect the HrSc by raising it (Figure 1). Thus, these two parameters are interrelated. The current investigation was performed to assess relationships between the programmed LRL, the HrSc, and survival.
Table 1: Multivariate analyses of variables associated with survival in a CRT-D population (n=67929) adapted from reference [3].
| Parameter | Hazard Ratio | P-value |
|---|---|---|
| Heart Rate Score/10% increase | 1.07 | <.0001 |
| LRL/10 bpm increase | 1.07 | <.0001 |
| Age/5 year increase | 1.18 | <.0001 |
| Gender (Male vs Female) | 0.74 | <.0001 |
| LV Pacing >98% vs <98% | 0.78 | <.0001 |
| Atrial fibrillation episode >24 hours prior to first histogram [1] | 1.12 | 0.01 |
CRT-D subjects enrolled from 2006-2011 as part of the ALTITUDE database that was monitored regularly via the LATITUDE® remote patient monitoring system (RPM) were included. The ALTITUDE database is a de-identified database of remote device transmission, approved by a Boston Scientific governance board, for deidentified investigation. The device remote transmissions are also used in product safety assessment. The LRL for these devices was programmed in increments of 5 ppm from 40-85 ppm. Classification of the LRL group was based on the predominant LRL programming during the first 6 months of RPM follow-up; 92% maintained a constant LRL throughout follow-up. HrSc was calculated at the first LATITUDE upload, usually in the first 45 days post-implantation.
A total of 71,059 subjects having a CRT-D implant, were monitored remotely and were included in the ALTITUDE database. Patients (n=9061) with persistent atrial fibrillation (AF) were excluded as the ventricular rate was not determined by atrial pacing or sensing; 117 were excluded because LRL programming was <40 or ≥90, as patients with this programming were too few for analysis. The remaining 61,881 patients were followed for up to 5 (mean 2.9) years. Surprisingly, >90% of subjects had LRL programming that differed from nominal (45 ppm), and 53% had LRL programming at 60 ppm.
The main finding was that lower LRL programming was associated with greater survival over the range of LRL 40-85 (log-rank p<0.0001). Patients with LRL programming >60 ppm were older, more likely male, more frequently programmed with rate-response “on”; and more frequently had a high HrSc (i.e., ≥70%). Accordingly, statistical corrections for risk factors were made. In a multivariate analysis correcting for these risk factors, higher LRL was associated independently with a greater risk of death when considering three HrSc groups: 1. low-risk HrSc<30%, 2. mid risk 30-70%, and high risk >70%. LRL programming at 80 or 85 ppm was both associated with poorer survival regardless of HrSc. The survival benefit of low LRL (<60 ppm) was greatest in subjects with a low HrSc (Figure 2). 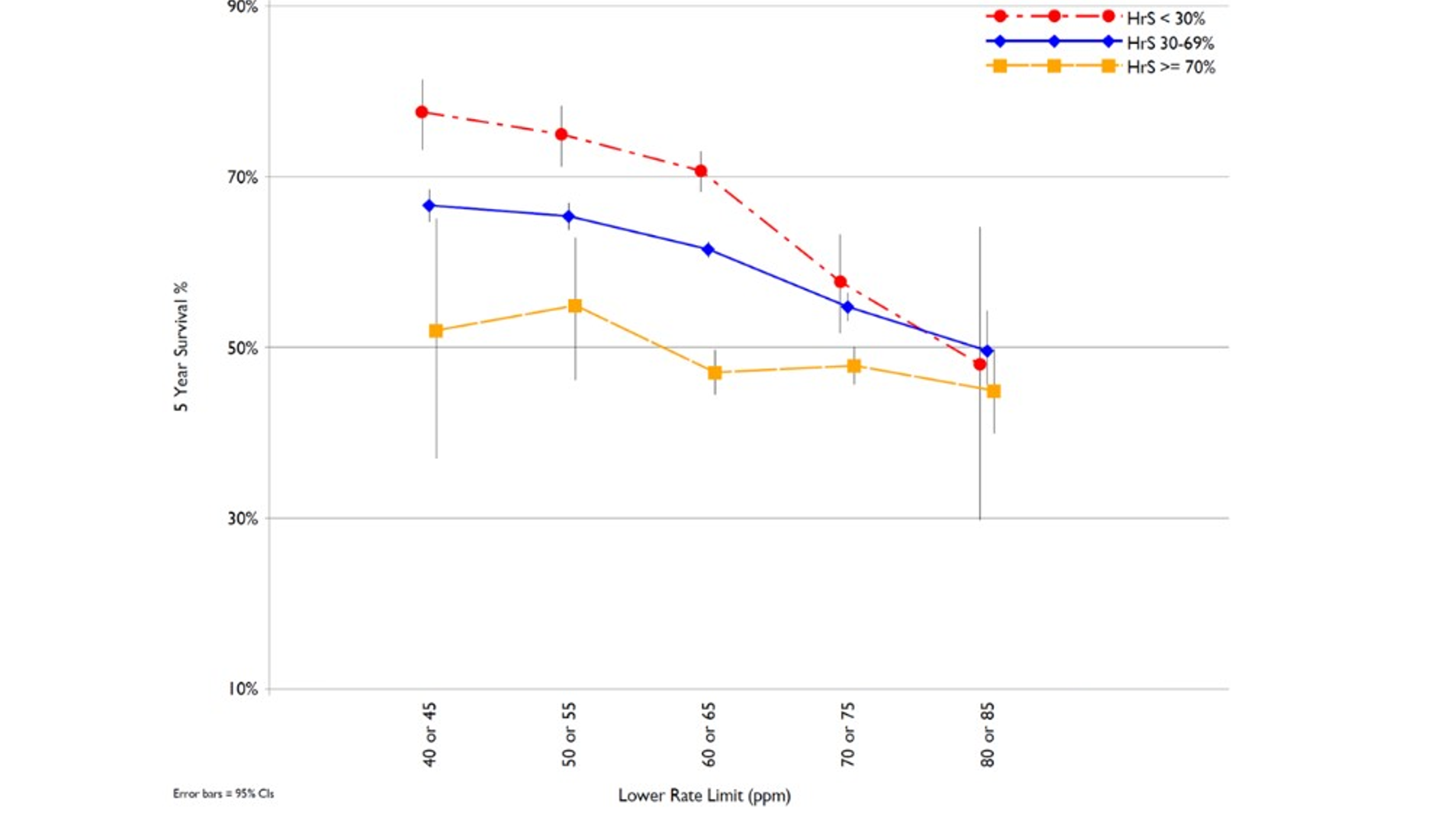
Figure 2: The 5-year survival percentage for the programmed LRLs 40 to 85 in five groups, and plotted for Heart Rate Score <30%, 30-69%, and ≥70%. The greatest association of lower rate programming with survival is in subjects with lower Heart Rate Scores (arrows). Adapted from reference [1].
Discussion
The major finding of this study is that a lower LRL was associated independently with better survival in this large CRT-D population over a five-year follow-up. HrSc and LRL were both associated with survival and, while HrSc and LRL were associated, there was a greater association between LRL and survival in the low HrSc versus the high HrSc group (Figure 2).
Why have prior randomized trials, such as PEGASUS-CRT [4] failed to show the benefit of lower LRL programming? One potential reason is that the heart rates in the groups programmed to lower LRL were not observed to subsequently have lower rates in the PEGASUS-CRT trial. That is, all groups had similar resting ventricular rates of about 70/min on follow-up electrocardiograms, regardless of LRL 40 or 70ppm. Similarly, rate histograms in the PEGASUS trial also did not show many differences between the study groups. This is in contrast to the marked differences seen in the “real world” data recently analyzed (Sharma AD, et al. (2021) [1], where lower LRL is associated with rate histograms with significant numbers of beats down to the LRL. Lower rates may occur with chronotropic incompetence or with adequate pharmacologic therapy (beta-blockers or ivabradine). Prior studies have shown that higher HrSc>70% are related to chronotropic incompetence in pacemaker subjects [5] and that CRT-D subjects with HrSc≥70% show survival benefit with rate-responsive pacing (DDDR-60) versus propensity score-matched DDD-60 subjects [6]. However, the current study showed that at HrSc≥70%, lower LRL had less impact on survival (Figure 2). This suggests a dual strategy of lower LRL in HrSc<70% subjects, and rate response (DDDR-60) for HrSc>70% subjects to maximize survival.
The majority of subjects in the ALTITUDE (“Real World”) database are programmed to LRL=60 suggesting that there may be the potential for significant survival benefits for select subjects with programming a lower LRL. Furthermore, this “real world” data shows a significant number of subjects are programmed chronically to LRL 70-85, a range of rates where there is no survival benefit observed.
Large databases such as this, have the advantage of being able to detect small differences because of the large numbers. This database also represents a better view of programming outside of clinical trials. However, this database has very limited clinical parameters, and as a result, we do not know the clinical basis for the selections of LRL in the “real world”. Accordingly, these findings will require further prospective controlled studies in selected subjects (HrSc<70%) to validate the observations and drive changes to clinical practice. These observations also do not necessarily pertain to transient changes in LRL programming, for example during acute heart failure decompensation, or pacemaker programming in subjects without heart failure. Similar future work is also needed to assess other pacing parameters, such as the upper rate limit.
Conclusion
Increased five-year survival in the order of 15-30% in CRT-D subjects is associated independently with slower LRL programming (<60ppm). A lower LRL is associated with lower HrSc, and thus HrSc and LRL do interact. At HrSc≥70% there is less survival benefit to lower LRL programming. These data suggest that further analyses and trials to assess the effect of LRL programming on survival in subsets of heart failure patients are merited, particularly in subjects with chronotropic incompetence and HrSc<70%.
References
1. Sharma AD, Wilkoff BL, Richards M, Wold N, Jones P, Perschbacher D, Olshansky B. Lower rate limit for pacing by cardiac resynchronization defibrillators: Should lower rate programming be reconsidered?. Heart Rhythm. 2021 Dec 1;18(12):2087-93. https://doi.org/10.1016/j.hrthm.2021.07.068
2. Olshansky B, Day JD, Moore S, Gering L, Rosenbaum M, McGuire M, Brown S, Lerew DR. Is dual-chamber programming inferior to single-chamber programming in an implantable cardioverter-defibrillator? Results of the INTRINSIC RV (Inhibition of Unnecessary RV Pacing With AVSH in ICDs) study. Circulation. 2007 Jan 2;115(1):9-16. https://doi.org/10.1161/CIRCULATIONAHA.106.629428
3. Wilkoff BL, Richards M, Sharma A, Wold N, Jones P, Perschbacher D, Olshansky B. A device histogram?based simple predictor of mortality risk in ICD and CRT?D patients: the Heart Rate Score. Pacing and Clinical Electrophysiology. 2017 Apr;40(4):333-43. https://doi.org/10.1111/pace.13036
4. Martin, D.O., Day, J.D., Lai, P.Y.. Murphy, AL., Nayak, H.M., Villareal, R.P., Weiner, S.V., Kraus, S.K., Martin DO, Day JD, Lai PY, Murphy AL, Nayak HM, Villareal RP, Weiner S, Kraus SM, Stolen KQ, Gold MR. Atrial support pacing in heart failure: results from the multicenter PEGASUS CRT trial. Journal of Cardiovascular Electrophysiology. 2012 Dec;23(12):1317-25. https://doi.org/10.1111/j.1540-8167.2012.02402.x
5. Richards M, Olshansky B, Sharma AD, Wold N, Jones P, Perschbacher D, Wilkoff BL. Addition of minute ventilation to rate-response pacing improves heart rate score more than accelerometer alone. Heart Rhythm. 2018 Nov 1;15(11):1730-5. https://doi.org/10.1016/j.hrthm.2018.06.021
6. Olshansky B, Richards M, Sharma A, Wold N, Jones P, Perschbacher D, Wilkoff BL. Survival after rate-responsive programming in patients with cardiac resynchronization therapy-defibrillator implants is associated with a novel parameter: the heart rate score. Circulation: Arrhythmia and Electrophysiology. 2016 Aug;9(8):e003806. https://doi.org/10.1161/CIRCEP.115.003806
